My Next Steps on Healing Through Nutrition

Summary: Over the years, the author has transformed her diet after discovering intolerances to dairy and gluten, which affected her mood. With a dietitian’s help, she focused on regular meals, balanced proportions, and healthy fats to manage weight and stabilise blood sugars. Now, addressing shoulder pain, the author has adopted a stricter anti-inflammatory diet for two weeks, cutting out sugar, most fruits, certain cooking methods, red meat, and dairy.
A lot has happened in terms of my nutrition over the last couple of years. I thought I would take some time to go through what has happened and where I am now with food.
Challenges with Gluten and Dairy
Working With A Dietician
Then, I started working with a dietician. I am overweight and, whilst I like the shape of my body as it is, I understand that the more fat reserves I possess, the higher my insulin needs are due to the insulin resistance the fat promotes. Therefore, I worked with a dietician with a view to releasing excess weight. We worked together for eight months. During that time, I overhauled my food. Some of the changes I made were:
-
I wasn’t completely reliable at eating breakfast, lunch and dinner each day. I changed that. I now eat regularly to nourish my body for the demands of my life.
-
My blood sugars were raising and then lowering quite substantially with every meal. We talked about insulin timing (I now aim to inject 20 minutes before each meal as this is the timing that works for me). We also looked at the order in which I eat the food on my plate. My dietician advised me to eat the vegetables first, then the protein, then the carbohydrates. This produces a much flatter curve to the meal.
-
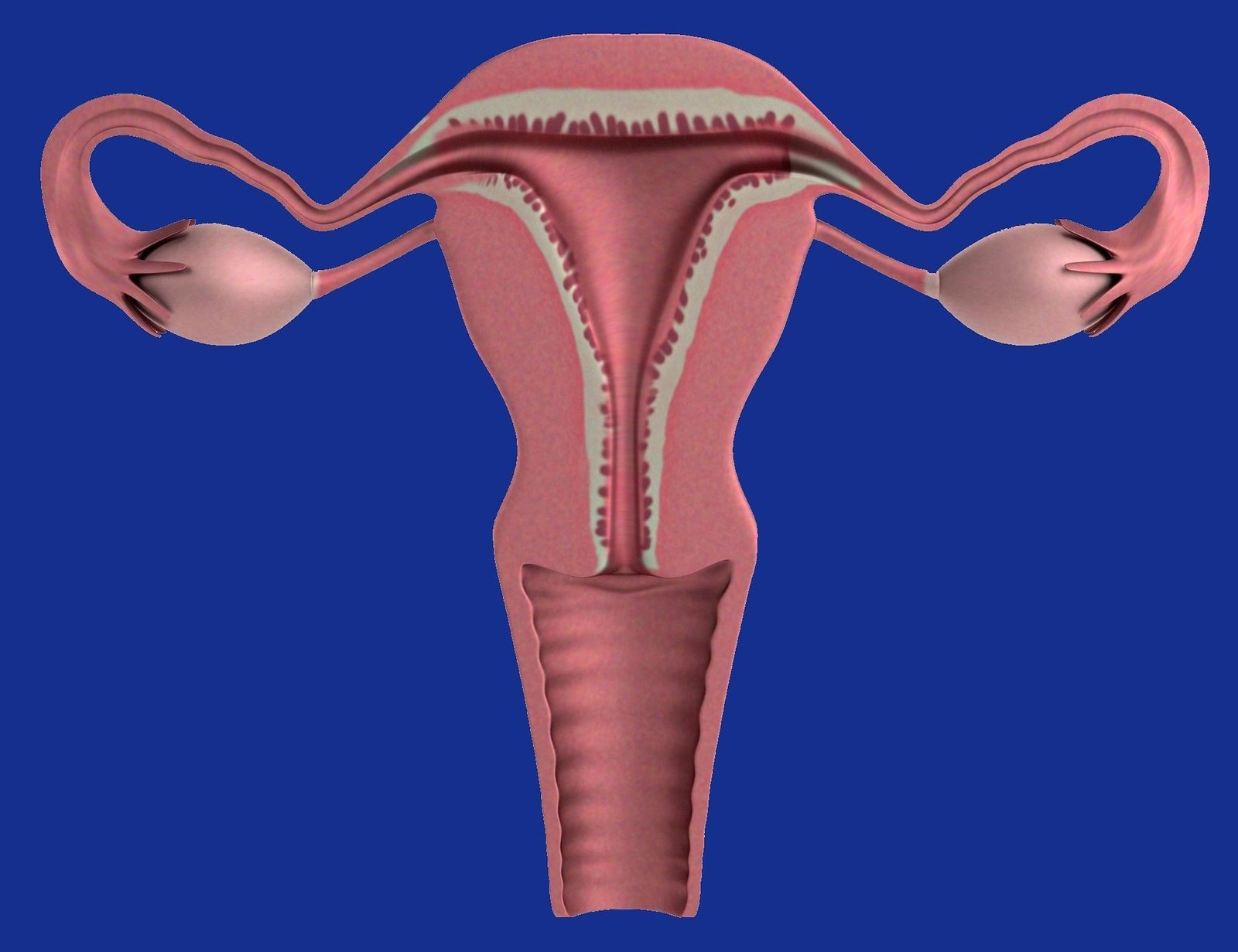
My dietician and I talked about the components of the meal. Each meal needs to be made up of a half a plate of vegetables or salad, then a quarter is protein and a quarter is a healthy carbohydrate. For now, visually measuring this is enough.
-
We discussed the importance of having healthy sources of fat in my diet. Fat is important for a multitude of reasons. These include being necessary for brain health, keeping blood pressure healthy, enabling you to absorb nutrients, and supporting cell growth. Also, fat keeps you satisfied and satiated. So adding some olive oil to your salad, or eating some avocado with breakfast, is much more likely to keep you away from the snack jar.
-
We talked about meal timing. We worked out that, for me, with my timetable and my nutritional needs, breakfast at 7-8am, lunch at 12pm, a mid-afternoon snack at 3-4pm and dinner at 6-7pm worked for me. (Please note: snacks are still a challenge. It brings me back to the forced snacks of my childhood that I had to eat whether I wanted it or not, just to stabilise blood sugars).
The Arrival Of Shoulder Pain
1. No sweets, chocolate or processed sugar.
2. No fruit, except for blueberries.
3. Vegetables can only be grilled or sautéed (not boiled or steamed)
4. No red meat, no seafood and no dairy. Only chicken and white fish.
5. Gluten-free bread (but it has to be toasted).
6. No foods or drinks that are too warm or too cold.

GET HEALINGT1D’S FUTURE ARTICLES IN YOUR INBOX!
Get the latest musings and findings straight to your email inbox.

Natalie is a blogger with Type 1 Diabetes. Natalie’s special gifts are questioning the status quo and being a rebel. She is using these gifts to question medical ‘knowledge’ and find a true cure for Type 1 Diabetes.











Recent Comments: