PCOS And Its Improvement Over Time
Summary: Today’s post focusses on something relevant to those who identify as female: the menstrual cycle. The author discusses Type 1 Diabetes and menstrual cycles, including recounting struggles with PCOS, including severe symptoms that significantly improved over time, possibly due to pregnancy and enhanced insulin sensitivity.
I was shocked to find out today (thanks to this journal article) that the rate of Type 1 Diabetes is 1.8 times higher in those that are biologically male than it is in those that are biologically female. I guess, having grown up in a family with Type 1 Diabetes just in the female line, I had a bit of a gender bias with my assumption here. I thought that the split would be at least even between the genders. I have been corrected! So, this article may not apply to a fair percentage of people reading this blog but, for those that it does, I feel it’s really important to write.
Today, I am talking about Type 1 Diabetes and the menstrual cycle. I haven’t exactly had an easy time of things in this area during my lifetime. My periods arrived late (something that is not uncommon in those with Type 1 Diabetes **ARTICLE**). This led to several visits to a gynaecologist, who diagnosed me with Polycystic Ovarian Syndrome (again, not uncommon in Type 1 Diabetes **ARTICLE**). Then, the fun really started. The periods that I had became almost unbearable. The highlights included:
- bleeding that lasted two weeks straight
- so much blood that I once had to stay on the toilet for fives days straight
- irregular bleeds (something else that is much more common in people with Type 1 Diabetes)
- years without periods
- and such out of control emotions that, whilst in a premenstrual period, I screamed so badly at one of my school friends that she never spoke to me again.
Not fun. Looking back on that time now, I believe that a fair amount of the dramatic symptoms I had could be linked to, or directly attributed to, my Polycystic Ovarian Syndrome (PCOS).
Healing Polycystic Ovarian Syndrome
At the time of diagnosis, it was explained to me that PCOS is an incurable condition. So I battled on with the symptoms, took birth control to regulate myself and shrugged my shoulders about my lot in life. Well, now I don’t have PCOS. I had a scan a couple of years ago for an unrelated issue and was told that I did not have it. There are no cysts on my ovaries at all and my ovaries are a normal size. Of course, at that time, I was told that I must have been misdiagnosed the first time around. (I didn’t ask the consultant at this time if I had also been misdiagnosed at the second, third, fourth, fifth, sixth and seventh scans and also during all of my pre-pregnancy planning with my medical team!).
I still have some excess facial hair but, beyond that, I have nothing to report. My periods are regular (I mostly have a 28 to 30 day cycle each month). The only exception to this is when I am particularly stressed out, which results in higher insulin levels and more insulin for my system. I have no excessive symptoms throughout my cycle – no pain, no cramping, no excessive bleeding, no other disruptions or inconveniences.
What Do I Believe Healed My Polycystic Ovarian Syndrome?
I think it was two things. Firstly, I believe that getting pregnant really helped. I remember once hearing Victoria Beckham (yep, the Spice Girl) once say that her PCOS healed when she had her first baby, Brooklyn. I think there’s something about pregnancy that presses the reset button on the female reproductive system. So there’s that. But that’s not exactly convenient for those that would like to get rid of their PCOS without the long-term commitment of raising a human to adulthood! So…
What factors contributed to this increased sensitivity? Essentially, everything I do to promote a healthier and happier lifestyle. These practices, which I extensively discuss on my blog, enhance my overall well-being. Unsure where to begin? Start with something that resonates with you. Avoid adding stress by forcing activities you don’t genuinely want to do, as stress exacerbates insulin resistance.
Type 1 Diabetes with a Regular(ish) Menstrual Cycle
Now that I am on a regular 28- to 30-day cycle, I still have challenges with varying insulin resistance at times. This has become even more clear to me since I have eliminated the gluten and dairy. Both gluten and dairy were triggering inflammation in my system and, as I have been banging on about for ages, inflammation causes insulin resistance… Just think of how much more insulin you have when you have the flu or tonsillitis or any other such lovely. After all, that’s what the sick day rules of diabetes were created for!
Now that I have eliminated the gluten and dairy, it has become more obvious to me that there are more predictable fluctuations in my insulin needs over the course of each menstrual cycle. Even with insulin resistance in the mix, I was already aware of the need for extra insulin during the week before my period (when I say more, I mean DOUBLE!). However, more subtle variations are now becoming more evident. To understand this in context, I’m going first need to divert for a moment to talk about the various phases of the menstrual cycle.
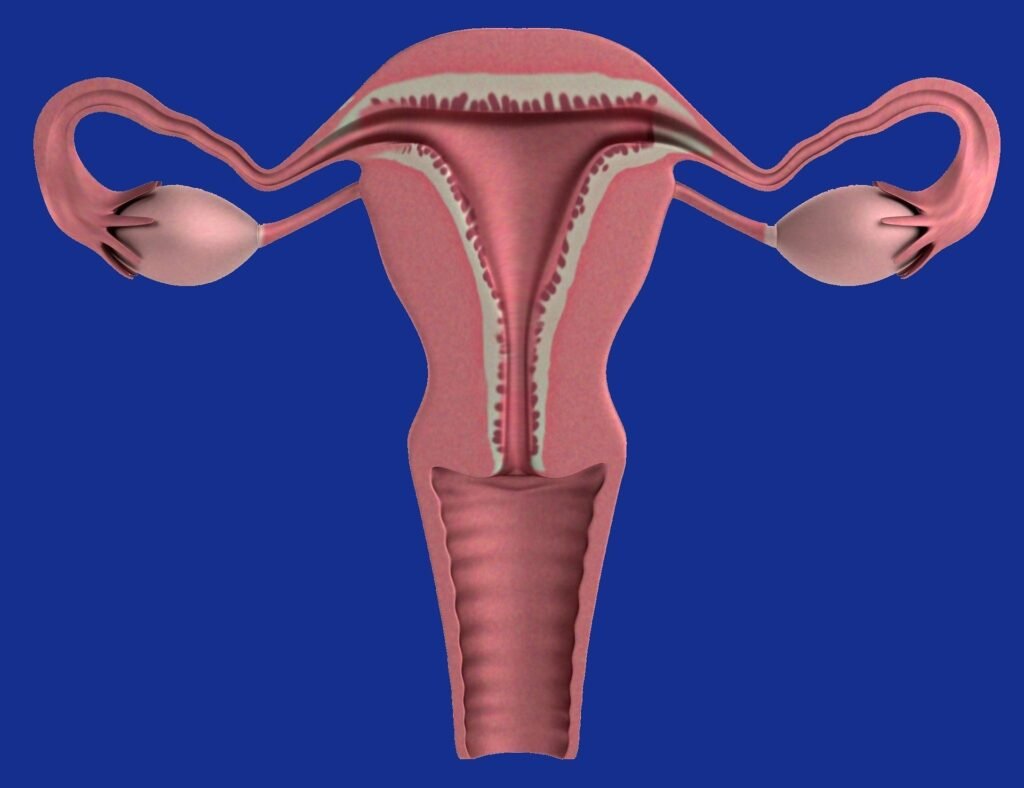
The Four Phases Of The Menstrual Cycle
A healthy menstrual cycle consists of four main phases. Whilst every woman is different and one woman’s periods can fluctuate in duration from one month to the next, the following is a guide of what the phases of the menstrual cycle may look like:
Days 1-5: Menstruation Phase
This is the ‘time of the month’ when the uterus lets go of its lining and a blood flow is observed. This bleed usually lasts for between three and seven days each month. Levels of oestrogen and progesterone are at their lowest levels during this phase of the menstrual cycle.
Days 6-14: Follicular Phase
During this phase, the uterus builds a thick lining in preparation for receiving the ovum (or egg) that will be released from the ovary in the coming days. In this phase, oestrogen typically rises whilst progesterone levels stay low.
Days 15-19: Ovulatory Phase
It is during this phase that an ovum is developed and then released into the uterus, ready to be fertilised by an sperm that are present. Both oestrogen and progesterone rise during this phase, peaking at the time just before ovulation.
Days 20-28: Luteal Phase
Assuming the ovum is not fertilised by a sperm, at this point the lining of the uterus is shed and the levels of oestrogen and progesterone fall back down to their lowest levels, preparing the body for menstruation.
Varying Insulin Resistance Caused by Oestrogen and Progesterone
In terms of blood sugar levels during the menstrual cycle, there are two key players that affect insulin resistance. These are oestrogen and progesterone. oestrogen is understood to decrease insulin resistance (increase insulin sensitivity). Progesterone is understood to increase insulin resistance (decrease insulin sensitivity). So, with fluctuating levels of BOTH of these hormones during the entirety of the menstrual cycle, less predictable blood sugar readings are to be expected. Here is what I have found:
Day 1 of my period: My insulin resistance dramatically switches off sometime during this day. My insulin requirement halves. It’s hard not to end up with an unexpected hypo (or elevated blood sugars for a large part of the day) with this unpredictable switch.
Days 2 – 4: my insulin sensitivity is high. I need half to two-thirds of my ‘usual’ Novorapid doses. Hypos are not unexpected territory here.
Days 5-8: usual insulin sensitivity (and therefore blood sugar control) is resumed.
Days 11-14: somewhere in this mix, my insulin requirements increase. This is in-line with the release of the ovum. This release increases two hormones LH and FSH, which are known to cause brief periods of insulin resistance.
Days 15-23: my blood sugars are stable here and my insulin requirements are in the normal range.
Days 24-28: my insulin resistance is THROUGH THE ROOF! I need more bolus (double!) and basal insulin. I also appear to be more sensitive to carbohydrates… My body reacts sharply and dramatically to any carbohydrates I eat. The progesterone is by far the biggest player in this blood sugar pattern, with the lowering effect of the oestrogen appearing to be insignificant or absent in my case. I also have strong carbohydrate cravings at this time. I believe these cravings are due to my body not being able to access the glucose already in my bloodstream because my insulin levels are not sufficient as a result of the dramatic insulin resistance. Nice Catch-22 there!
I have learnt that my period pattern is substantiated in the medical literature. As an example, Barata et al. (2013) clearly demonstrated that blood sugar control is markedly different between the follicular and luteal phases, with more insulin being required in the latter half of the menstrual cycle.
I haven’t, as yet, got to the point where I can predict with any degree of certainty what insulin requirements I might have on each day of my cycle. It’s still a bit hit-and-miss. But, now having a clearer picture of what my cycle is doing and how my insulin requirements change over each few days of my cycle, I have more hope than I did. I will report back with what I learn!

GET HEALINGT1D’S FUTURE ARTICLES IN YOUR INBOX!
Get the latest musings and findings straight to your email inbox.

Natalie is a blogger with Type 1 Diabetes. Natalie's special gifts are questioning the status quo and being a rebel. She is using these gifts to question medical 'knowledge' and find a true cure for Type 1 Diabetes.
Recent Comments:
- Sandra on Nutrition Update
- latestModapks on Daniel Darkes
- Natalie Leader on Daniel Darkes
- Senna on Daniel Darkes
- Sandra on High Blood Pressure