Summary: The Eisenbarth model explains Type 1 Diabetes (T1D) as an autoimmune disease where the immune system targets and eliminates pancreatic beta cells, cells that are crucial for insulin production. However, recent research offers hope for treatment advancements and cure. Research has highlighted the potential for beta cell preservation and regeneration, including findings on delta cell transformation and the presence of dormant and baby beta cells in the pancreas.
After 38 years with diabetes, I felt pretty sure that I was the Mastermind champion on Type 1 Diabetes (T1D)!
I knew that my pancreas was defunct. Irreparable. Beyond salvation. Dead as a dodo.
Life with T1D
T1D management can be tricky and, at times, onerous. I maintain my T1D through testing my blood sugar levels up to ten times per day.
I inject insulin at each meal and at bedtime (see my ‘Insulin‘ post for further exploration on this topic).
I inject varying amounts of insulin for each meal. The amount depends on the carbohydrates on my plate (or, more accurately, in my stomach!!).
Insulin dosing is a fine art. Too much, I hypo (‘hypoglycaemia’). I become listless, confused and sometimes uncooperative. Too little insulin, my blood sugars run too high (‘hyperglycaemia’). I become irritable, anxious and sometimes mean.
But I am well and I am healthy. I live a full and active life. I am a wife to a non-diabetic husband. I am a mother to a non-diabetic child. I travel. I exercise. I live. I have fun.
The Finer Detail...
But I have to hang my head and say that I don’t TRULY know what diabetes is. I’ve heard about the islets of Langerhans. But I couldn’t explain to you what they are. I know that my beta cells have been attacked by my immune system. But I can’t draw you a picture of what that looks like. And I don’t know why my immune system attacked my beta cells to start with.

Back To School
I decided that the first stage of my healing process must include improving my knowledge levels. How could I slay the beast without knowing what it looked like? How could I understand what healing from T1D required if I didn’t know what its mechanism actually was?
In healthy individuals, the immune system is so advanced that it is able to differentiate between pathogens and the normally functioning cells, tissues and organs of the human body.
The dominant model to explain diabetes is the Eisenbarth model [1]. This model states that T1D is a chronic autoimmune disease where the immune system attacks the pancreatic beta cells. It mistakenly identifies the beta cells in the pancreas as pathogens and sets about eliminating them [2].
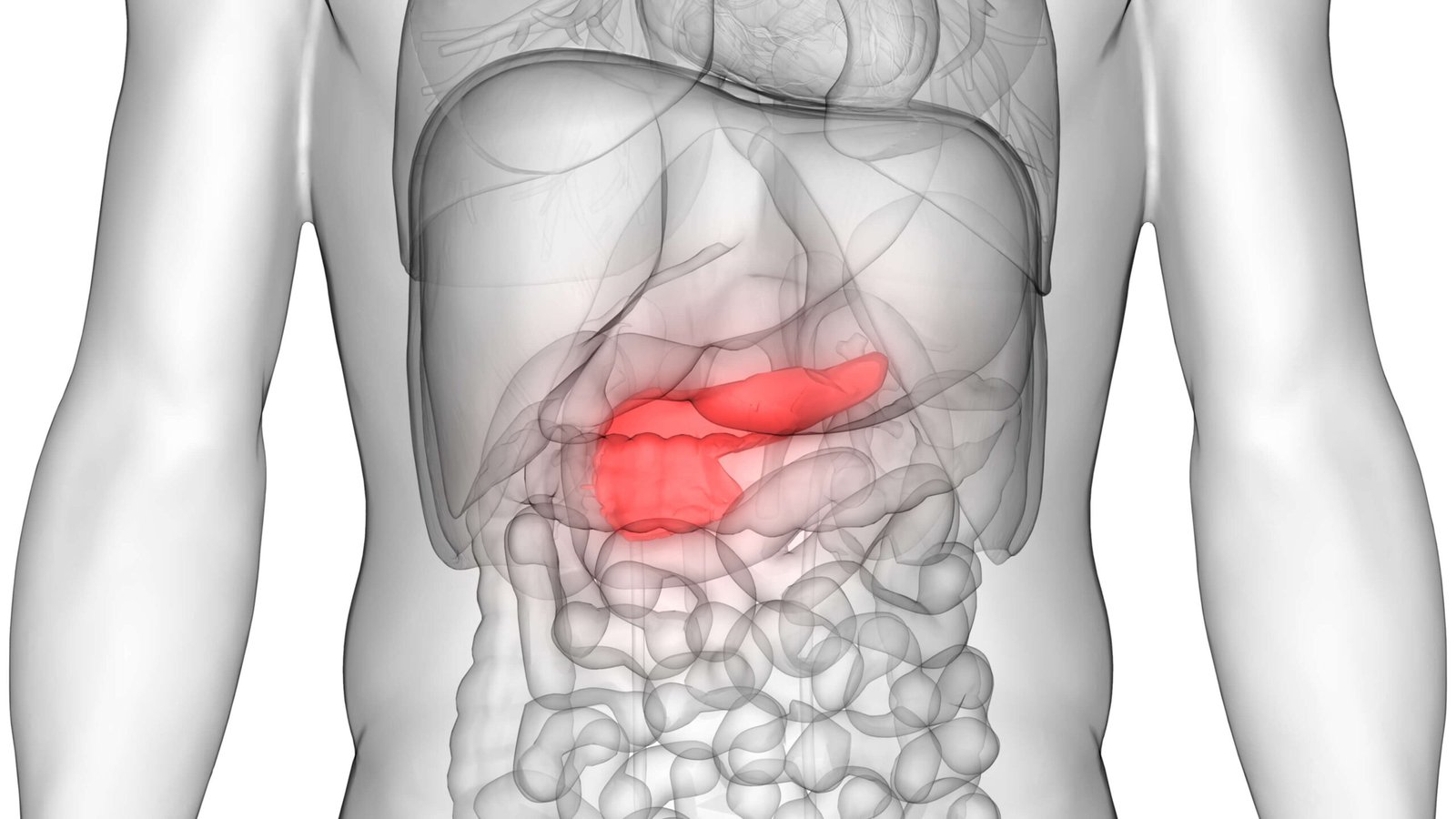
The Pancreas
So here it is, the little beauty! What strikes me most about this organ is how unnoticed AND unnoticeable it is! If you ask most healthy people, they could describe where the major organs of the brain, heart, lungs, kidneys, stomach, bladder and bowel are located. But the pancreas…?
The pancreas is part of the digestive system. It is conveniently situated behind the stomach. It has both endocrine and exocrine functions. The endocrine functions are mostly focussed on regulating blood sugar levels. It achieves this by secreting a series of hormones, including insulin, straight into the bloodstream. The exocrine functions involve supplying the stomach with digestive enzymes. These enzymes break food down into carbohydrates, proteins and fats.
What Are Beta Cells?
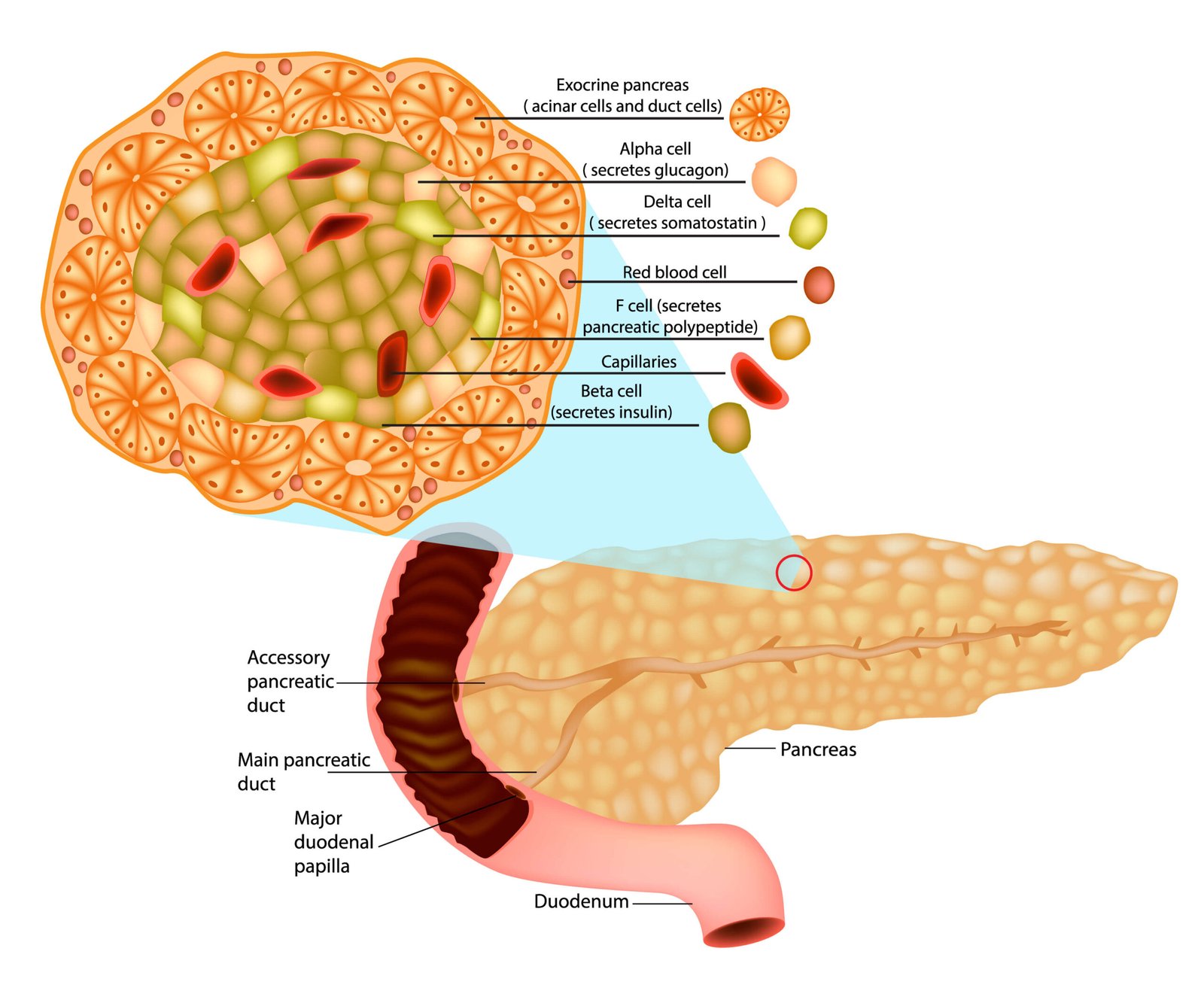
There are three types of endocrine cells:
- Alpha Cells: secrete glucagon. Glucagon is responsible for stimulating the liver to convert glycogen stores into ready-to-use glucose.
- Beta Cells: secrete insulin.
- Delta Cells: produce somatostatin that inhibits the secretion of glucagon and insulin.
All three are found in the pancreatic islets. These pancreatic islets are also known as the ‘islets of Langerhans’. These were named after the German anatomist Paul Langerhans, who discovered them in 1869.
Researchers generally posit that T1D occurs when the majority (between 70-90%) of the beta cells have been destroyed [3], [4], [5], [6]. Without these beta cells, the pancreas is unable to produce enough insulin to maintain healthy blood sugar levels.
Beta Cell Mass and Beta Cell Function
Now this is where, for me, things got a bit more murky. More recent research [8] suggests that the lack of sufficient insulin in diabetes could in fact result from two different factors:
- Reduced beta cell mass: there are fewer working beta cells in the pancreas due to increased beta cell death.
- Reduced beta cell function: the beta cells are still alive and well in the pancreas but they are in a dormant/non-functioning state.
So which one is relevant to Type 1 Diabetes? It would appear that the answer is… BOTH! For T1D that developed before the age of 14, there appears to be a higher number of inflamed islets (suggesting a reduction in their functioning) and also a lower number of remaining beta cells [9]. For T1D developed in the teenage years, however, beta cell mass is still surprisingly high [10]. The beta cells are still there, just not working right! It is thought that the marked increase in the loss of beta cell mass in the early years of Type 1 Diabetes is due to an increased level of the inflammatory process ‘insulitis’ [10].
Why Were My Beta Cells Inhibited And/Or Destroyed?
I have millions of cells in my body that do thousands of different jobs so why on earth did my rampaging, rebellious, body-wide immune system choose to turn in on my beta cells? That’s pretty specific! Why not the cells responsible for producing nasal mucus (that’s snot and bogeys to you and me!!)? I’d prefer to do without those!
Well, now the next piece of the story unravels… It turns out that the immune system in T1D may actually be working perfectly. Instead, it is the beta cells that become dysfunctional [11]. This dysfunction causes the immune system to (quite correctly) identify them as pathogens, unhealthy to the system. It therefore sets about clearing them out.
Is All Hope Lost?
Secondly, research does not seem to support Eisenbarth’s proposal that great numbers of beta cells have been destroyed by the immune system… In fact, only modest increases in beta cell death have ever been found in T1D [13]. So the beta cells might not even be dead…?!
Instead, researchers [14] have demonstrated that the pancreas of T1Ds hold a larger-than-normal number of delta cells in their pancreas. Therefore, they suggest that, instead of the beta cells dying, they have been converted from insulin-producing beta cells into insulin-inhibiting delta cells. These same authors also found that this cell transformation is reversible, meaning that the delta cells can be changed back into fully-functioning beta cells under laboratory conditions.
Thirdly, it has been found that when beta cells from Type 2 Diabetics are taken out of the ‘stressful stimulus’ provided by their bodily environment, they started producing insulin again [15].
Fourthly, cutting-edge research has found that the pancreas has its own back-up system in place! Hidden in plain sight from researchers for over one hundred years is a population of baby beta cells tucked up around the edges of healthy pancreatic cells [16]. These baby cells can already produce some insulin. I therefore wonder if it’s possible to grow these into fully-functioning ‘adult’ beta cells to restore insulin production in the pancreas.
Hope Still Exists!
These four findings give me great hope. Although I do not have any measurable C-Peptide, I may still have dormant beta cells (which therefore are not producing C-Peptide). These may just need a wake-up call to get going again. However, even if I don’t have these dormant but healthy beta cells that can go forth and multiply, I still do have a source for creating new ones… The baby beta cells in the periphery of my pancreatic cells. Furthermore, the notion that the environment of the cell may inhibit insulin production makes me think about how I might change that environment myself to encourage beta cell proliferation.
Rebooting The Pancreatic Cells
So I need to find a way to reawaken my dormant beta cells (if I have any), and/or transform my delta cells back into fully-functioning beta cells and/or grow my baby beta cells into adult form. As I have discussed above, beta cells can suddenly start producing when the environment they are in is changed. This makes sense to me. After all, how do you get a plant or an infant to grow? You provide it with the right nutrition, environment and conditions for growth to take place.
In my forthcoming blog posts, I will further support and expand upon the thoughts in this post. Furthermore, I will be exploring a whole series of factors that I believe will contribute to the (re)growth of my beta cells.
Summary
- Type 1 Diabetes was originally understood to be an autoimmune disorder resulting from a misfiring immune system killing off the pancreatic cells that produce insulin (beta cells).
- The beta cells are stored in pancreatic islet cells, along with alpha cells (that secrete glucagon) and delta cells (that produce somatostatin, which inhibits insulin and glucagon production).
- Cutting-edge research is demonstrating that: i) the beta cells in the pancreas may not be destroyed after all; ii) beta cells have been transformed in the pancreas into insulin-inhibiting delta cells, which can be transformed back to beta cells; iii) changing the environment of inhibited beta cells can enable them to start producing insulin again; iv) the pancreas also contains baby beta cells that have the potential to develop into fully-functioning beta cells for those who do not have their own supply.
- T1D appears to be more healable than the ‘beta cells have been burnt out’ theory suggests.
Glossary:
Alpha Cells: one of three types of cells found in the pancreatic islets. These are responsible for releasing glucagon to raise low blood sugar levels.
Autoimmune disease: a disease caused by the immune system attacking cells or tissues in the human body that should not normally be attacked.
Beta Cells: one of three types of cells found in the pancreatic islets. These are responsible for producing insulin, which lowers blood sugar levels.
Beta Cell Function: a measure of the ability of the insulin-producing beta cells to produce insulin.
Beta Cell Mass: a measure of the number of fully-functioning beta cells remaining in the pancreas.
Blood sugar levels: a measure of the amount of glucose in the bloodstream. In diabetes, the body’s natural ability to maintain this at an optimum level is diminished.
Carbohydrates: sugars, starches and fibres that are found in food stuffs. Carbohydrates are normally the body’s main source of energy, being utilised to increase blood glucose levels as and when required.
Chronic: long-term.
C-Peptide: an amino acid produced concurrently with insulin in the pancreas. A detectable level of C-peptide in the bloodstream is indicative of insulin production in the pancreas.
Delta Cells: one of three types of cells found in the pancreatic islets. These are responsible for inhibiting the production of glucagon and insulin from the alpha and beta cells respectively.
Eisenbarth model of diabetes: the currently dominant model of diabetes used by the majority of researchers and doctors to explain how T1D occurs. It suggests that T1D results from the immune system attacking and breaking down the beta cells in the pancreas, thus causing hyperglycaemia.
Hyperglycaemia: the presence of too much sugar in the bloodstream.
Hypoglycaemia: the presence of too little sugar in the bloodstream.
Immune System: this is a complex, body-wide system that protects a body against pathogens and disease. It consists of many cells, organs and tissues of the anatomy.
Insulin: a hormone produced by the beta cells in the pancreas. It is responsible for lowering glucose levels in the bloodstream. In T1D, insufficient insulin is produced by the pancreas. The lacking insulin is replaced with external insulin, either via injection or insulin pump.
Insulitis: a disease of the pancreas where immune cells infiltrate the pancreatic islets, causing beta cell loss.
Islets of Langerhans: also known as pancreatic islets. Each one is a specific small area of the pancreas that contains three main cells that are responsible for producing hormones; alpha cells, beta cells and delta cells.
Pancreas: an organ of the body, situated behind the stomach. It has roles to play in both the digestion of food and regulation of blood sugar levels in the bloodstream. In T1D, one small part of the pancreas, the beta cells, no longer produce insulin.
Type 1 Diabetes (T1D): an autoimmune disease that occurs when the immune system attacks and destroys the insulin-producing beta cells in the pancreas.
References:
Pugliese, A., and Skyler, J. S. (2013). George S. Eisenbarth: Insulin and Type 1 Diabetes. Diabetes Care, 36(6), 1437-1442. [Article]
Holt, R. I. G., and Hanley, N. A. (2012). Essential Endocrinology and Diabetes. Chichester, UK and Hoboken, NJ: Wiley-Blackwell Publishers. [Book]
Gepts W. (1965). Pathologic anatomy of the pancreas in juvenile diabetes mellitus. Diabetes, 14(10), 619–633. [Article]
Gepts W., and De Mey J. (1978).Islet cell survival determined by morphology: An immunocytochemical study of the islets of Langerhans in juvenile diabetes mellitus. Diabetes, 27(S1), 251–261. [Article]
Junker K., Egeberg J., Kromann H., and Nerup J. (1977). An autopsy study of the islets of Langerhans in acute-onset juvenile diabetes mellitus. Acta Pathologica et Microbiologica Scandinavica. Section A, Pathology, 85(5), 699–706. [Article]
Kloppel G., Drenck C. R., Oberholzer M., and Heitz P. U. (1984). Morphometric evidence for a striking B-cell reduction at the clinical onset of type 1 diabetes. Virchows Archiv A Pathological Anatomy and Histopathology, 403(4), 441–452. [Article]
Chen, C. et al. (2017).Human Beta Cell Mass and Function in Diabetes: Recent Advances in Knowledge and Technologies to Understand Disease Pathogenesis. Molecular Metabolism, 6(9), 943-957. [Article]
Atkinson, M. A., von Herrath, M., Powers, A. C., and Clare-Salzler, M. (2015). Current Concepts on the Pathogenesis of Type 1 Diabetes — Considerations for Attempts to Prevent and Reverse the Disease. Diabetes Care, 38(6), 979-988. [Article]
Sims, E. K., and DiMeglio, L. A. (2019). Cause or effect? A review of clinical data demonstrating beta cell dysfunction prior to the clinical onset of type 1 diabetes. Molecular Metabolism, 27S, S129-S138. [Article]
Oram, R. A., Sims, E. K., and Evans-Molina, C. (2019). Beta cells in type 1 diabetes: mass and function; sleeping or dead? Diabetologia, 62(4), 567–577. [Article]
Butler A. E. et al. (2007).Modestly increased beta cell apoptosis but no increased beta cell replication in recent-onset type 1 diabetic patients who died of diabetic ketoacidosis. Diabetologia, 50(11), 2323–2331. [Article]
Piran, R., Lee, S. H., Li, C. R., Charbono, A., Bradley, L. M., and Levine, F. (2014). Pharmacological induction of pancreatic islet cell transdifferentiation: relevance to type I diabetes. Cell Death and Disease, 5, e1357. [Article]
Jeffery, N., et al. (2019).Cellular Stressors may alter islet hormone cell proportions by moderation of alternative splicing patterns. Available at: https://ore.exeter.ac.uk/ repository/ bitstre am/handle/10871/37184/Jeffery%20et %20al.,%20HMG%202019.pdf?sequence=1.
van der Meulen, T., et al. (2017).Virgin Beta Cells Persist throughout Life at a Neogenic Niche within Pancreatic Islets. Cell Metabolism, 25(4), 911-926. [Article]

GET HEALINGT1D’S FUTURE ARTICLES IN YOUR INBOX!
Get the latest musings and findings straight to your email inbox.

Natalie is a blogger with Type 1 Diabetes. Natalie's special gifts are questioning the status quo and being a rebel. She is using these gifts to question medical 'knowledge' and find a true cure for Type 1 Diabetes.
Recent Comments:
- Sandra on Nutrition Update
- latestModapks on Daniel Darkes
- Natalie Leader on Daniel Darkes
- Senna on Daniel Darkes
- Sandra on High Blood Pressure



5 responses to “What Is Type 1 Diabetes REALLY?”
Truly amazing information! I am determined to do the same, obviously being smart and healthy about it. We can do this and we got this!! Look forward to hearing about your progress!!
I have a question. What diet are you implementing? I have been struggling finding the correct diet for me. I am very active, workout a lot. I want to be in the best shape possible and work my way to helping awaken my beta cells as well. Any suggestions would be appreciated!
Hi Jeromy,
Thank you for your comments! I wish you luck with your healing journey… Please be careful. Diabetes is a serious condition that always deserves respect.
Regarding diet, I am aiming to eat as naturally as possible. I think that reducing the number of toxins (pesticides, highly processed foods etc) cannot do harm and may potentially do good. I think the most important thing is to listen to your body. What does your body need to heal? If you listen hard enough, it will tell you. I do not think following a prescribed dietary plan would work for me. But, if you feel that that will lead to you better health, then that is up to you to decide. Personally, I would try to reach for health rather than for a specific diet-related goal.
I hope you read this (sorry I just found this post)! I am of the same mind as you are concerning T1D reversibility! I have a 13 year old daughter diagnosed the hard way, DKA, almost 1 year ago. Following a path of healing we went from Dr. Bernstein’s methodology (low carb, learning to calculate proper insulin dosing with “Regular” insulin); to Dr. Jason Fung’s fasting addition; and finally to Dr. Annette Bosworth’s protocol where you actually measure your biochemistry AND a keto diet with fasting! She has seen major improvement with all types of metabolic disorders!! One word of major hope is: AUTOPHAGY!! I would LOVE to be in touch with you to get your thoughts and/or willingness to share information.
Sincerely, Diann
Hi Diann,
Thank you so much for reaching out on my blog! I am glad to hear that you guys are making such strides with your daughter’s healing. I followed Dr Bernstein myself for a while and had great results from it. I am also, like you, interested in the healing potential of autophagy. I have been keeping an eye on the work of Dr Jockers, who is a huge supporter of it. I’m just a bit wary myself because of a few published case studies I’ve read on Type 1 Diabetics ending up in diabetes ketoacidosis as a result of fasting, despite having normal blood sugars (see here for an example: https://www.ncbi.nlm.nih.gov/books/NBK554570/). I am therefore a bit cautious about it. On the other hand, I believe that each person’s health is completely individual and therefore fasting might cause issues in some but not in others. For me, at this time, I intuitively feel it is not a right choice for me but certainly will be revisiting the idea at a later date. I would love to hear about your daughter’s progress with it as time goes on! Best wishes till then.